Neural tube defects (Spinal Dysraphism) is the umbrella term for defects of the brain and spine that occur very early in pregnancy. The brain, spinal cord or bones of the spinal column at the back (spinal arch) fail to develop normally. Normally the spinal cord is a tubular structure that resides in a bag of fluid and is protected by a bony cage formed by the vertebral body and spinal arch. In neural tube defects there is failure of either the spinal cord going from a flat sheet to a tubular structure, failure of the bones to develop leaving a defect or “bifid spinal arch” or failure of the skin the develop leaving the spinal cord exposed. Neural tube defects can be further subdivided in to open defects (Spina Bifida aperta) where the spinal cord is exposed, with no skin cover and closed defects (Spina bifida occulta) where the defect is skin covered.
The stages of brain and spine development at which these entities occur , prognosis and management differ considerably. What most people are referring to when they are talking about Spina Bifida is the open defect. Here we will discuss the closed spinal dysraphism group of defects.
This group encompasses a wide range of defects which occur due to failure of disjunction or secondary neuralation in the development of the brain and spine. The common denominator is that they are all skin covered lesions of the lower spine that do not generally have any associated brain malformations. Most children are diagnosed after birth when either a fatty lump is noted on their lower back or other skin changes are noted over the spine. Babies may also be noted to have foot deformities that result in scans that ultimately reveal a closed dysraphic condition.
The vast majority of children do not have mobility problems in the first instance however these may develop as the child grows and tension develops on the spinal cord which in most cases is “low lying” or “tethered”. Normally the spinal cord ends at the level of the L1 vertebrae but this can be lower in children with closed spinal dysraphism. The same is often true of bladder and bowel function where most children will develop normal sphincter function initially.
There is a wide spectrum of conditions that fall under the closed dysraphism umbrella. These include
- Spinal Lipoma/Lipomyeloceles- fatty fibrous tissue attached to the spinal cord and extending through a gap in the spinal column attaching into the fat under the skin
- Dermal Sinus tracts- a persistent channel that connects the spinal cord directly to the skin (photos below)
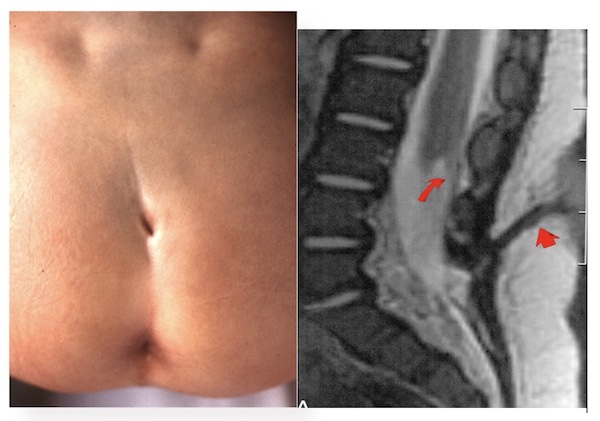
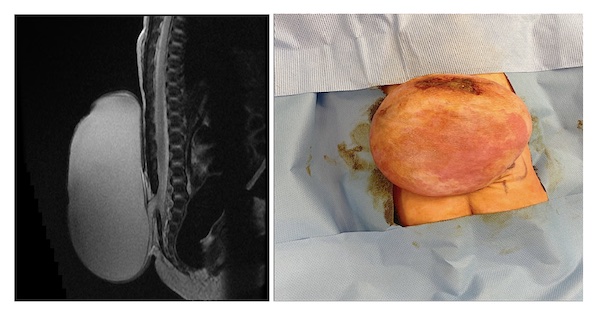
- Limited dorsal myeloschesis/Meningoceles-Sac of spinal fluid covered by skin. There can be nerve tissue within or lining the sac (photos below)
- Thickened or fatty filum -thickening of the band of tissue that connects the lower end of the spinal cord to the lower end of the thecal sac (the sack containing the spinal cord and spinal fluid
- Split cord malformations (diastematomyelia) (photos below)

- Caudal regression syndromes
- Neuroenteric cysts
If your child is referred without a scan, an MRI and kidney ultrasound is organised following which your child is reviewed at the Neuro-Urology clinic at CHI Temple Street.
In this clinic you will meet a Neurosurgeon and a Urology specialist along with our specialist nurses.
Most children will be managed expectantly with routine follow -up as they grow. Repeat scans +/- surgical intervention is offered if they develop symptoms of sphincter disturbance (bowel or bladder weakness), pain (back/leg pain), impaired mobility or evolving foot deformities. This is known as Tethered Cord Syndrome. Some lesions will require early surgical intervention eg. Dermal sinus tracts and certain lipomas.
Some children may require orthopaedic referral if they have significant foot deformities, tight tendons or gait difficulty.
If your child is showing signs of bladder dysfunction, they will go on to have this investigated with Uroflow +/- urodynamic tests and if necessary you will be trained in how to catheterise your child.
Children with closed dysraphism are generally follow-up up until they have completed their growth (generally up to the age of 16).
